When Telehealth Marketing Goes Too Far, Everyone Pays the Price
A note on perspective
Before getting into this, I want to be clear about how this article should be read.
This reflects my personal observations and interpretation as a founder operating in the telehealth space. I’m describing patterns I’m seeing and the concerns they raise for me. Reasonable people may disagree with those interpretations, and that disagreement is healthy.
This is not meant to be definitive. It is meant to be honest.
⸻
A note on intent
I also want to be explicit about what this article is not.
I am not referring to any specific company, product, or clinician, and I am not alleging wrongdoing. This is not an accusation. It is a broader concern about incentives, optics, and how legislative responses tend to unfold when healthcare categories drift toward consumer excess.
With that context in place, here’s what I’m seeing — and why it worries me.
⸻
The real concern isn’t innovation. It’s incentive distortion.
Telehealth has made real healthcare more accessible for millions of people. That includes sexual health, STI prevention, and treatment for conditions like erectile dysfunction. These are legitimate medical needs, and telehealth has helped reduce stigma, cost, and geographic barriers.
But there is a meaningful difference between using telehealth to expand access to care and using prescription medication primarily as a marketing device to sell subscriptions.
Increasingly, based on what I’m seeing, large, well-funded telehealth companies appear to be pushing hard against that line.
The concern isn’t hypothetical. If this arms race continues, the likely outcome isn’t just questionable advertising. It is greater legislative scrutiny, tighter statutory rules, and ultimately fewer options for patients who rely on telehealth for legitimate care.
To be clear, many of these products may be offered within existing legal frameworks. The issue isn’t legality alone. It’s whether the way prescription authority is being used and promoted still aligns with the medical intent behind it.
⸻
The rise of “lifestyle medications”
Recently, I’ve been seeing advertisements for caffeinated drinks combined with prescription erectile dysfunction medication.
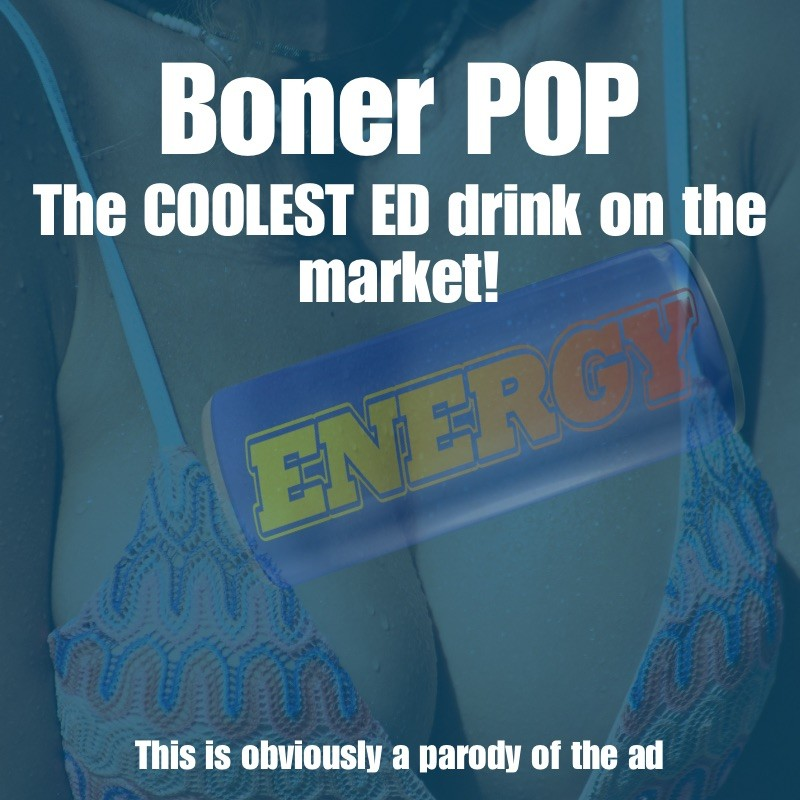
This isn’t a theoretical example. It’s something that shows up regularly in my social media feeds.
On paper, these products appear to be offered legally. Patients are evaluated. Prescriptions are issued. The medication is compounded by a pharmacy based on a physician’s order.
But legality does not automatically equal medical appropriateness.
Erectile dysfunction medications are prescription-only because they alter blood flow and can have meaningful cardiovascular effects. Caffeine is a stimulant that raises heart rate and blood pressure. There may be hypothetical clinical scenarios where combining these substances could be justified for a specific patient.
But that’s not how I see these products being marketed in the advertising I encounter.
From what I’m observing, they are not typically framed as:
- Treatment for a clearly defined medical condition
- Therapy for a specific, well-described patient population
- A carefully balanced intervention for a documented use case
Instead, they are often presented as a cool drink that makes sex better.
That distinction matters.
⸻
How compounded medications are intended to work
To understand why this distinction is important, it helps to understand how compounding is intended to function.
When a doctor prescribes a compounded medication, they are not selecting a premade product. They are issuing a custom prescription, specifying each ingredient and its dose.
For example:
Sildenafil X mg
Caffeine Y mg
The compounding pharmacy prepares exactly what the physician orders.
This framework exists to help patients who:
- Need nonstandard doses
- Cannot tolerate commercially available formulations
- Require alternative delivery methods
- Have allergies or contraindications
Compounding is meant to address individual medical needs, not to create consumer-facing lifestyle products.
When ingredients are combined primarily for appeal or novelty, rather than to address a specific clinical requirement, the broader compounding ecosystem becomes more vulnerable to scrutiny.
⸻
Where telehealth access is actually decided
In practice, state legislatures, not medical boards, are the entities that ultimately make or break telehealth access.
Legislatures decide:
- Whether telehealth prescribing is permitted
- Which medications may be prescribed remotely
- Whether synchronous video visits are required
- Whether in-person exams must precede certain prescriptions
- How compounding and mail-order fulfillment are treated under state law
These decisions are often driven by public pressure, media narratives, and perceived overreach, not by careful distinctions between responsible and irresponsible actors.
There is precedent for this.
In the past, some states took a conservative approach to telehealth prescribing. For example, South Carolina’s telemedicine statute once included a prohibition on remote prescribing of “lifestyle medications” such as erectile dysfunction drugs unless specifically authorized by the medical board, which effectively limited access for patients relying on telemedicine for care. That prohibition has since been removed as part of telehealth modernization efforts, but it illustrates how legislative reactions to telemedicine practices can create access barriers when prescription drugs begin looking like consumer products rather than medical treatments.
When legislatures respond, they do so broadly. They do not draft laws that distinguish between:
- Careful providers and aggressive marketers
- Evidence-based use and novelty-driven formulations
Statutes apply to everyone.
⸻
Marketing vs medicine is a legislative fault line
Legislators are not clinicians. They evaluate healthcare policy largely through:
- Public testimony
- Advertising examples
- Media coverage
- Consumer complaints
When prescription medications are presented in ways that resemble:
- Energy drinks
- Lifestyle enhancers
- Consumer packaged goods
It becomes easier to frame telehealth as something that needs to be “reined in.”
Historically, when lawmakers perceive that a category has drifted from medical seriousness into consumer excess, the response is restriction, not nuance.
⸻
Why subscription models amplify legislative risk
Subscription-based healthcare models change incentives in ways that are visible from the outside.
When revenue depends on continuous consumption, pressure can shift from:
“Does this patient need this medication?”
to:
“How do we keep patients engaged month after month?”
Even if clinicians act responsibly, the appearance of the model matters in legislative settings.
From the outside, these systems can begin to resemble:
- Recurring product sales
- Consumption-driven prescribing
- Lifestyle optimization rather than treatment
That perception alone is often enough to trigger policy responses.
⸻
A thought experiment
Imagine if antibiotics were marketed the same way.
Picture a daily caffeine-based drink containing doxycycline, branded as:
“Max Power Defense”
“Just drink one a day and your STI risk drops by 80%!”
Even if the underlying science were sound, the framing alone would likely provoke legislative backlash.
Not because doxycycline is ineffective, but because medical nuance disappears when medications are presented as lifestyle beverages.
⸻
What’s actually at stake
Telehealth earned public and legislative trust by being serious, restrained, and purpose-driven.
If telehealth becomes widely associated with:
- Viral ads
- Trend-driven formulations
- Prescription drugs marketed like consumer beverages
Legislative responses are likely to follow.
Those responses may include:
- Narrower telehealth prescribing authority
- Mandatory in-person visit requirements
- Restrictions on compounding
- Higher compliance burdens for everyone
When that happens, the people who pay the price are not companies.
They are patients who lose access.
⸻
Why Shameless Care took a different approach
Shameless Care was not built around subscriptions. That was a deliberate choice.
We built this company because it was extraordinarily difficult for people to access:
- Thorough STI testing
- Evidence-based prevention
- Honest sexual healthcare without gimmicks
Our focus has always been on:
- Clear medical indications
- Clinical appropriateness
- Transparency over novelty
Revenue should follow trust, not precede it.
⸻
The bottom line
Telehealth is powerful. Compounding is powerful. But both rely on legislative trust as much as clinical trust.
When prescription medications are reframed as lifestyle products, legislative scrutiny becomes more likely. And when laws change, they change broadly.
Healthcare innovation doesn’t require abandoning medical seriousness.
If anything, it depends on protecting it.
Get valuable knowledge like this, straight to your inbox once a week.
No spam, no sales pitches. Just knowledge. Unsubscribe any time, and we’ll never sell your information.